Minimally Invasive Total Hip Replacement
All muscles are preserved during surgery
Anterior Approach
Muscle sparing hip replacement
General information
Muscle sparing
No muscles are detached
It is important to be well informed before taking the decision to undergo a muscle sparing hip replacement. The better informed you are, the easier the rehabilitation after surgery will be. A hip replacement is indicated when the hip pain can no longer be controlled by other measures such as painkillers, injections or lifestyle modifications. The most frequent reason why a hip replacement is needed is due to arthrosis of the hip (coxarthrosis). Arthrosis means that the protective cartilage layer has been worn down. Other common reasons why surgery might be necessary are avascular necrosis of the hip (reduced blood supply), hip dysplasia or rheumatoid arthritis.

Doorsnede door de heup
The direct anterior (muscle-sparing) approach uses a natural pathway or interval between the muscles at the front of the hip. The incision is 10 to 15cm and is positioned anteriorly on the leg, instead of on the side (lateral approach), or in the gluteal region (posterior approach). Superficially the interval runs in between the Sartorius and the Tensor Fascia Lata muscles. More deeply, the interval runs in between the gluteal muscles (Gluteus Medius and Minimus) and the Rectus Femoris.
Due to the fact that no muscles are being cut during surgery, the initial rehabilitation is quicker compared to the more traditional lateral or posterior approach. In fact this newer technique often allows walking on the new hip, on the same day of the surgery. The need for crutches is usually shorter and the length of hospital stay can be reduced to 3 or 4 days.
Another advantage is that the risk of dislocation of the hip replacement is very limited. During surgery the patient is positioned supine (lying on the back) which makes it easier to ensure the correct leg length, compared with the traditional side-lying position. In fact, a significant leg length difference after surgery is extremely rare when using this technique.
No muscles are being cut during surgery, but muscles do have to be pulled out of the way. This may (mainly in men) result in some pain in the thigh the first few days after surgery. This usually disappears after 3 or 4 days. Painkillers and regular applications of ice are helpful.
The lateral femoral cutaneous nerve (LFCN) is a sensory nerve that runs close to the skin incision. In about a third of cases the lateral side of the thigh can feel slightly numb after surgery. This usually disappears over the course of a couple weeks. In rare cases this can result in a painful sensation at touch (Meralgia Paresthetica).
In theory the anterior approach can be used in every individual. However, in some cases the surgeon might suggest another approach. For example, when previous incisions are present, if there are skin lesions or for revision surgery in cases with complex anatomy, due to previous hip trauma or surgery.
Types of hip replacements

There are different types of hip replacements:
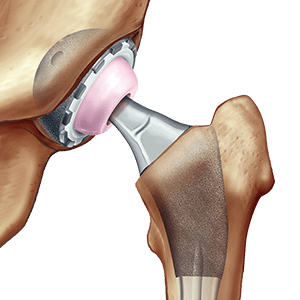
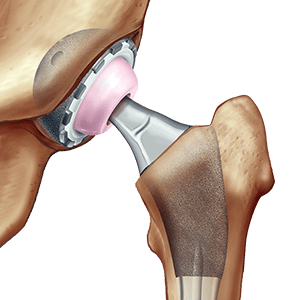
- A total hip replacement: The acetabulum (on the pelvic side) and the femoral head (on the thigh bone) are both replaced. The acetabular component is called the “cup” and the component in the thigh bone is called the “stem”. This is by far the most commonly used type of hip replacement.
- The bipolar hip replacement: In this case the acetabulum is not being replaced. This type of replacement has its limitation and is only indicated in frail and elderly patients who sustain a hip fracture.
Materials
Different materials can be used during a total hip replacement. Important factors are age and level of existing bone quality.
Both the cup and the stem are made of titanium. This biocompatible material is very strong and ideal for ingrowth in the bone. Rejection or allergy to this metal is extremely rare.


Ceramics for medical use have very low wear rates. The head of the hip replacements are nearly always made of ceramics. The inside of the cup, called the “liner”, can also be made of ceramics. This is mainly used in patients younger than 50 years of age.
Polyethylene is a hard type of plastic. The inside of the cup (the liner) can be made of this material. This is the standard in patients older than 60 years of age.

Depending on the bone quality, a total hip replacement can be fully cementless. This means that both the cup and the stem are being fixed to the bone without the use of cement. In a primary hip replacement, the cup will always be uncemented. The bone will grow onto the rough surfaces of the titanium implants. If necessary additional screws can be used for primary stability. In most cases a cementless stem can also be used. However, in case of low bone quality due to age or osteoporosis, a cemented stem may be recommended.
Before Surgery
Before
Preoperative consultation
Before a surgery can be planned a couple of preoperative checks must be completed.
- Preoperative consultation with the anaesthetist: Surgery is performed under general anaesthesia. The anaesthetist will review any current medication. Routinely an ECG and a blood analysis will be performed. If necessary additional investigations may be required.
- Preoperative templating radiograph: A pelvic X-ray with a calibration marker is used to digitally template the correct size of the hip replacement.
- In case of dental problems it is important to have this treated before hip surgery. During dental procedures, bacteria may enter in the blood and potentially cause an infection of the hip replacement, which can lead to complications.
Information session
Every month information sessions are organised at the Gasthuisberg Hospital. The entire team (surgeon, nurse, physiotherapist, social worker) will explain the procedure extensively and describe the rehabilitation after surgery. These sessions are held in Dutch language. The dates can be found here.
Skin and nasal decontamination
Infection of a hip prosthesis can be caused by bacteria that can commonly be found on the skin. To decrease the risk of infection, you will have to use a decontaminating soap starting 5 days prior to admission. The prescriptions and instructions for use will be provided during the preoperative clinic.
Get fit for surgery!
Smoking cessation

Smokers have a strongly increased risk of complications after surgery: E.g. wound problems, infection of the prosthesis, ingrowth problems, pulmonary embolism, venous thrombosis, myocardial infarction. It is absolutely necessary to quit smoking at least 2 months before surgery.
Weight loss

Obesity is a also strong predictor of postoperative complications (specifically infection and wound healing problems). Other complications such as pulmonary embolism and thrombosis can also occur much more frequently. It is important to achieve a healthy weight before surgery. Ideally the Body Mass Index would be less than 40.
It has been recognized that patients tend not to lose weight after surgery, even if activity is generally increased. Therefore a healthy weight must be achieved before surgery.
Discharge?
Prepare for rehab
Get in touch with a physiotherapist of your choice who can treat you after surgery.
Practice how to walk with crutches and how to do transfers before your surgery. A link to the instructional videos can be found here.
Prepare your discharge
You will be able to leave the hospital on average 3 to 4 days after surgery. Plan in advance where you will be staying for your rehab. If you decide to stay in a rehab center, this needs to be planned well in advance. Please get in touch with the social worker if you need any assistance: contact social worker.
Day of surgery
Admission
Admission is at 7 am the day of surgery. Patients who are planned to be operated first in the morning may be admitted on the evening before surgery. You have to be nil-by-mouth (no food/milk) from midnight before surgery. Drinking of water only is allowed until 4 hours before surgery.
Anesthesia
The procedure routinely takes place under a general anaesthetic. If this is contraindicated, a locoregional anaesthesia (spinal) can alternatively be used.
At the end of the surgery additional local anaesthetic agents are injected into the wound for pain control during the first hours after surgery.
Surgery
First you will enter the preparation room, where an intravenous line will be put in. After completing all the checks, you will be transported to the operating theatre. The anaesthetist will take care of the general anaesthetic and monitor you throughout the surgery. The procedure normally takes 1h to 1h15 on average. After surgery you will be woken up and monitored in the recovery room for 2 hours.
Where is the incision?

Normal incision

Bikini-incision
A longitudinal incision is routinely used. Depending on personal preference also a “bikini” incision can be used.
Hospital stay
After surgery
After the procedure
- A local anaesthetic will be administered in the wound at the end of the surgery. This decreases the pain during the first hours after surgery. However, towards the end of the day, the local anaesthetic may wear off. It is therefore very important not to skip any painkillers, even if the pain is well controlled at that specific moment.
- Drink plenty of water
- Move your feet and legs. A pillow will be placed in between the legs until the morning after surgery. However, you should not keep your legs still during that time. Move both your feet and bend your knee till your foot is flat on the bed.
- If you feel well enough the physiotherapist will get you out of bed in the afternoon and help you to take the first steps on your new hip.
Day 1 after surgery
- Blood analysis to control blood loss (haemoglobin)
- Removal of intravenous line after administration of last dose of antibiotics
- If a drain was used, this will be removed in the morning.
- The dressing stays on.
- Swelling around the wound is normal.
- You will walk in your room or the corridor with a walking frame or with 2 crutches
- Ice application and rest after the exercises will reduce pain and swelling.
- In men the entire thigh can often feel very stiff.
- A slight increase in temperature (up to 38.5°) is normal the first 2 or 3 days after surgery.
- In the evening, you will receive a subcutaneous injection for thrombosis prophylaxis. This is changed to oral medication on discharge.
Day 2 after surgery
- An x-ray of the hip and pelvis is performed to check the position of the replacement.
- Physiotherapy: walking with crutches in corridor and exercises in the physio room.
- Men can often still suffer from pain and stiffness in the thigh: maintaining enough movement and physio is crucial.
- Continue ice applications and rest after the exercises.
- Return to home is possible if all discharge criteria have been fulfilled.
Day 3 after surgery
- The physiotherapy exercises will be increased. Climbing stairs with crutches will be performed today.
- The dressing will be changed to a transparent dressing before discharge.
- Discharge if the criteria are met.
Discharge criteria
You are medically fit to leave the hospital if:
- The wound is dry and clean.
- The pain is well controlled on oral medication.
- The physiotherapy goals have been achieved: Safe walking with crutches, transfers & using stairs.
The exact day of discharge strongly varies from person to person and depends on your age, general health, the severity of the arthrosis and the preoperative muscle status. The average length of stay in the hospital is 3 to 4 days.
Back home
Important
First weeks after surgery
Your physiotherapist will follow you up during your rehabilitation at home. Specific instructions regarding mobilisation and weight-bearing will be found on the physiotherapy prescription. Usually 2 crutches have to be used for 4 weeks postoperatively to reduce the risks of falling.
It is normal to have some muscle pain the first weeks after surgery. Remember to rest after the exercises and take a pain killer if necessary. Do not forget to apply ice 3 times daily.
Swelling of the leg is normal and will gradually migrate toward the knee. This will then disappear after a couple weeks.
In up to 30% of the cases, a numb feeling might be present on the lateral (outer) side of the leg. This will slowly decrease, but it may take several weeks or months.
If there are any problems with the wound (discharge, bleeding, redness) you should immediately contact the hospital.
Medication
- Blood thinning medication will be prescribed to prevent deep venous thrombosis (DVT). This can consist of daily injections or, in most cases, oral medication (Xarelto ™), for 30 days after surgery.
- Anti-inflammatory drugs are prescribed during 2 weeks to prevent calcifications in the muscles and to decrease pain and swelling. These should always be taken with a meal and must be stopped in case of gastrointestinal intolerance.
- As mentioned previously, pain is normal the first weeks after surgery. Take enough painkillers so it remains possible to do all of the exercises.
Compression stockings
Compression stockings are not necessary after an anterior hip replacement. They are only prescribed if you have a history of thrombosis or an otherwise increased risk. Swelling of the leg is normal after surgery, but remaining active will help to increase circulation and decrease the swelling.
Nursing follow-up at home
- A transparent and water-resistant dressing will be applied on the wound before discharge. This dressing does not need to be changed daily. If the dressing comes loose, a nurse should be asked to reapply this. The sutures are reabsorbable and only the knots on the side have to be removed by your GP 2 – 3 weeks after surgery. The suture itself does not have to be removed.
- If necessary a nurse can offer daily help with getting dressed or washing. A prescription will be provided by the assistant on the ward.
Follow up
Follow-up appointments
- At 6 weeks: Clinic with radiographic control (x-ray). The position of the components and wound healing are checked.
- At 1 year: Clinic with X-ray control. Assessment of bony ingrowth of the hip replacement.
- Further follow-up depending on the symptoms.
Monitoring the quality of our care
Monitoring the quality of our care is one of the priorities of the University Hospitals of Leuven. You will be asked to fill out questionnaires on a regular basis. This will help us to follow your rehabilitation process and allow us to improve the care for our future patients.
At the moment we our using the online MoveUp Platform for data collection. Please find more information here.
Complications
Alarming signs:
Please contact immediately the Orthopaedic department of the University Hospitals of Leuven if you have one of the following symptoms or clinical signs.
Contact details:
8u – 17u: Secretary of the orthopaedic department: 016/338827
17u – 8u: Emergency care: Oncall orthopaedic doctor: 016/343900
Late complications:
As with any other surgery, there are certain risks associated with the placement of a hip replacement and complications are possible. The risks of developing one of these complications is very low:
- Infection of the hip replacement: in most cases a reoperation (wash-out or replacement of the prosthesis) will be necessary. Antibiotics are always administered during surgery to minimise this risk.
- Dislocation: this means that the femoral head comes out of the cup of the prosthesis. It can occur after a fall or due to extreme rotational movements. During your hospital stay, the physiotherapist will teach you how to avoid these movements. The risk of dislocation is highest in the first 3 months following surgery.
- Periprosthetic fracture is a fracture of the bone around the hip replacement. This usually happens after a fall and in most cases surgery is necessary. If the hip replacement is still fixed to the bone it can be maintained, however if the replacement is loose it will have to be changed.
F.A.Q.
How long does a hip replacement last?
Most hip replacements will last 15 to 20 years. Registry studies show a prothesis survival of 95% at 15 years and 85-90% at 20 years. This depends on several factors such as age, weight, level of activity and severity of deformations before surgery.
Due to increased quality of the materials used for hip replacements, problems such as loosening and wear & tear are becoming increasingly rare. Fractures, dislocation and infection on the other hand are becoming more frequent in the aging population.
Sports
It is definitely feasible to do sports with a hip replacement. The main concern is falling, which is a risk for dislocation and fracture. Sports such as walking, cycling, golf and swimming are recommended. More intensive sports such as jogging, tennis and skiing are often also possible.
Certain sports are not recommended: martial arts, football, rugby,…
Always discuss your return to sports with your physician.
Sleeping?
The first night after surgery you will have to sleep on your back with a pillow in between your legs. From the second night on, you can sleep in any preferred position. The most comfortable positions are usually on the back or on the side of the operation. If you want to sleep on the non-operated side, it is often more comfortable to put a pillow between the legs.
Driving?
There are no strict rules about driving after surgery. We recommend waiting until 6 weeks after surgery. At the first postoperative follow-up clinic your physician will check whether or not you are able to drive again.
Travelling?
Metal detectors at airports may detect the presence of metal implants such as hip and knee replacements. There are no official certificates available to prove the presence of a medical implant.
If you are planning to fly the first month after surgery, this will have to be discussed with your surgeon as the risk of thrombosis may be increased.
Antibiotics?
Always mention you have undergone a hip replacement when other surgeries are planned. Certain procedures (dental procedure, colonoscopy,…) can cause a hematogenous infection of a hip replacement. This means that during these procedures, bacteria from the bowel or mouth can enter the bloodstream and go on to infect the prosthesis. To avoid this, the use of prophylactic antibiotics is recommended the first 2 years after your hip replacement.
Oral hygiene
Good oral hygiene is important before you undergo a hip replacement to decrease the risk of infection. If necessary a dental check-up should be performed before the hip replacement is performed.
Return to work?
The exact time of return to work depends on the type of work being performed. Most office jobs can be resumed after 6 weeks. However, it will be difficult to stay seated for more than a few hours. For heavy manual labor, return to work is often only possible after 3 months.
Sexual relations
People who undergo total hip replacement often experience difficulties in sexual intercourse due to
pain or stiffness of the hip. After surgery the mobility of the hip will start to improve and the pain will
lessen, making sex pleasurable again for both partners.
However, caution is advised during the first 6 weeks after the procedure. The wound should heal
nicely and bear in mind the internal scar tissue is also formed during this period. During this first
phase of rehabilitation, a number of guidelines must be followed. In general, extreme bending
movements combined with twisting movements should be avoided and the patient should adopt a
more passive position (see illustration). As soon as the hip has healed properly, a more active role
can be played and these restrictions should be relaxed.
You can always ask your surgeon, nurse or physiotherapist if you have further questions.